On February 28, 1998, the revered British medical journal The Lancet published a brief paper by then-high profile but controversial gastroenterologist Andrew Wakefield that claimed to have linked the MMR (measles, mumps and rubella) vaccine with regressive autism and inflammation of the colon in a small case number of children. A subsequent paper published four years later claimed to have isolated the strain of attenuated measles virus used in the MMR vaccine in the colons of autistic children through a polymerase chain reaction (PCR amplification). The effect on vaccination rates in the UK was immediate, with MMR vaccinations reaching a record low in 2003/2004, and parts of London losing herd immunity with vaccination rates of 62%. 15 American states currently have immunization rates below the recommended 90% threshold. Wakefield was eventually exposed as a scientific fraud and an opportunist trying to cash in on people’s fears with ‘alternative clinics’ and pre-planned a ‘safe’ vaccine of his own before the Lancet paper was ever published. Even the 12 children in his study turned out to have been selectively referred by parents convinced of a link between the MMR vaccine and their children’s autism. The original Lancet paper was retracted and Wakefield was stripped of his medical license. By that point, irreparable damage had been done that may take decades to reverse.
How could a single fraudulent scientific paper, unable to be replicated or validated by the medical community, cause such widespread panic? How could it influence legions of otherwise rational parents to not vaccinate their children against devastating, preventable diseases, at a cost of millions of dollars in treatment and worse yet, unnecessary child fatalities? And why, despite all evidence to the contrary, have people remained adamant in their beliefs that vaccines are responsible for harming otherwise healthy children, whether through autism or other insidious side effects? In his brilliant, timely, meticulously-researched book The Panic Virus, author Seth Mnookin disseminates the aggregate effect of media coverage, echo chamber information exchange, cognitive biases and the desperate anguish of autism parents as fuel for the recent anti-vaccine movement. In doing so, he retraces the triumphs and missteps in the history of vaccines, examines the social impact of rejecting the scientific method in a more broad perspective, and ways that this current utterly preventable public health crisis can be avoided in future scenarios. A review of The Panic Virus, an enthusiastic ScriptPhD.com Editor’s Selection, follows below.
Such fervent controversy over inoculating young children for communicable diseases might have seemed unimaginable to the pre-vaccine generations. It wasn’t long ago, Mnookin chronicles, that death and suffering at the hands of diseases like polio and small pox were the accepted norm. In 18th Century Europe, for example, 400,000 people per year regularly died of small pox, and it caused one third of all cases of blindness. So desperate were people to avoid the illnesses’ ravages, that crude, rudimentary inoculation methods were employed, even at the high risk of death, to achieve life-long immunity. A 1916 polio outbreak in New York City, with fatality rates between 20 and 25 percent, frayed nerves and public health infrastructure to the point of near-anarchy. As the disease waxed and waned in outbreaks throughout the decades that followed, distraught parents had no idea about how to protect their children, who were often far more susceptible to fatality than adults. By the time Jonas Salk’s polio vaccine breakthrough was announced as “safe, effective and potent” on April 12, 1955, pandemonium broke out. “Air raid sirens were set off,” Mnookin writes. “Traffic lights blinked red; churches’ bells rang; grown men and women wept; schoolchildren observed a moment of silence.” Salk’s discovery was hailed as “one of the greatest events in the history of medicine.”

Mnookin doesn’t let scientists off the hook where vaccines are concerned, however, and rightfully so. Starting around World War II, with advances such as the cowpox and polio vaccines, along with the dawning of the Antibiotics Age, eradicating death and suffering from communicable diseases and bacterial infections, a hubris and sense of superiority began to creep into the scientific establishment, with dangerous consequences. Fearing the threat of biological warfare during World War II, a 1941 hastily-constructed US military campaign to vaccinate all US troops against yellow fever resulted in batches contaminated with Hepatitis B, resulting in 300,000 infections and 60 deaths. The first iteration of Salk’s polio vaccine was only 60-90% effective before being perfected and eventually replaced by the more effective Sabin vaccine. Furthermore, dozens of children who had received doses from the first batch of vaccines were paralyzed or killed due to contaminated vaccines that had failed safety tests. In 1976, buoyed by the death of a soldier from a flu virus that bore striking genetic similarity to the 1918 Spanish flu epidemic strain, President Gerald Ford instituted a nation-wide mass vaccination initiative against a “swine flu” epidemic. Unfortunately, although 40 million Americans were vaccinated in three months, 500 developed symptoms of Guillain-Barré syndrome (30 died), seven times higher than would normally be expected as a rare side effect of vaccination. Many people feel that the scars of the 1976 fiasco have incurred a permanent distrust of the medical establishment and have haunted public health influenza immunization efforts to this day.
These black marks on the otherwise miraculous, life-saving history of vaccine development not only instilled a gradual mistrust in public health officials, but laid the groundwork for the incendiary autism-vaccine scandal. The only missing components were a proper context of panic, a snake oil salesman and a compliant media willing to spread his erroneous message.
Enter the autism epidemic and Andrew Wakefield’s hoax. Because this seminal event had such a profound effect on the formation and proliferation of the current anti-vaccine movement, it is chronicled in far greater detail than our introduction above. From precursor incidents that ripened the potential for coercion to the Wakefield’s shoddy methodology and the naive medical community that took him at his word, Mnookin weaves through this case with well-researched scientific facts, interesting interviews and logic. A large chunk of the book is ultimately devoted to the psychology of what the anti-vaccine movement really is: a cognitive bias and a willingness to stay adamant in the belief that vaccines cause harm despite all evidence to the contrary. “If you assume,” he writes, “as I had, that human beings are fundamentally logical creatures, this obsessive preoccupation with a theory that has for all intents and purposes been disproved is hard to fathom. But when it comes to decisions around emotionally charged topics, logic often takes a back seat to a set of unconscious mechanisms that convince us that it is our feelings about a situation and not the facts that represent the truth.”
Given this blog’s objective to cover science and technology in entertainment and media, it would be disingenuous to write about the anti-vaccine movement without recognizing the implicit role played by the media and entertainment industries in exacerbating the polemic. By lending a voice to the anti-vaccine argument, even in a subtle manner or in a journalistic attempt to “be fair to the other side,” over time, an echo chamber of lies turned into an inferno. In 1982, an hour-long NBC documentary called DPT: Vaccine Roulette aired, overemphasizing rare side effects in babies from vaccinations to a nation of alarmed parents and completely undermining their benefits. It was a propaganda piece, but an important hallmark for what would come later. A 2008 episode of the popular ABC hit show Eli Stone irresponsibly aired anti-vaccination propaganda involving a lawyer questioning a pharmaceutical company that manufactures vaccines due to the even then-debunked link to autism. For several recent years, actress and Playboy bunny Jenny McCarthy (who is given an entire chapter by Mnookin) became a tireless advocate against vaccinations, believing that they gave her son autism. She didn’t have any scientific proof for this, but was nevertheless given a platform by everyone from Larry King on CNN to a fawning Oprah Winfrey.

As it turns out, McCarthy’s son never even had autism, but rather a very rare and treatable neurological disorder. In a self-penned editorial for the Chicago Sun-Times, she has officially retroactively denied her anti-vaccine stance, and says she simply wants “more research on their effectiveness.” An extremely sympathetic 2014 eight-page Washington Post magazine article profile of prominent anti-vaccine activist Robert F. Kennedy, Jr. (who believes in the link between vaccines and autism) repeated his talking points numerous times throughout. This, among an endless cycle of interviews and appearances by defiant anti-vaccine proponents, given equal air time side-by-side with frustrated scientists, as if both positions were somehow viable, and worthy of journalistic debate. Once the worm was out of the can, no amount of rational discourse could temper the visceral antipathy that had been created. This is irresponsible, dangerous and flat-out wrong. When the public is confused about an esoteric issue pertaining to science, medicine or technology, influencers in the public eye cannot perpetuate misinformation.
Despite the unanimous medical repudiation of Wakefield’s fraudulent methods and conclusions and the retraction of his Lancet paper, an irreversible and insidious myth had begun permeating, first among the autism community, then spreading to proponents of organic and holistic approaches to health and finally, to mainstream society. In the aftermath of the controversy, epidemiological studies debunking the autism-vaccination “link,” combined with a growing disease crisis, have forced the largest US-based autism advocacy organization to reverse its stance and fully endorse vaccination to a still-divided community. Wakefield remains more defiant than ever, insisting to this day that his research was valid, attempting to sue the British journalism outlet that funded the inquiry into his fraud and peddling holistic treatments for autism as well as his “alternative” vaccine. Sadly, the public health ramifications have nothing short of disastrous, with a dangerous recurrence of several major childhood diseases.
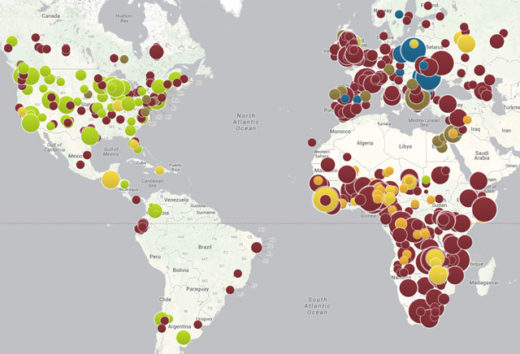
A few examples of the many systemic casualties of the anti-vaccination movement (many occurring just since the publication of Mnookin’s book):
•A summary from the American Medical Association about the nascence of the measles crisis in 2011, when the US saw more measles cases than it had in 15 years
•Immunization rates falling so low that schools in some communities are being forced to terminate personal exemption waivers and, in some cases, legally mandated immunization for public school attendance
•California’s worst whooping cough epidemic in 70 years.
•Most recently, a measles outbreak at Disneyland, resulting in 26 cases spread across four states, after an unvaccinated woman visited the theme park
•Anti-vaccine hysteria has spread to Europe, which has had a measles rise of 348% from 2013 to 2014 (and growing), along with an alarming resurgence of pertussis
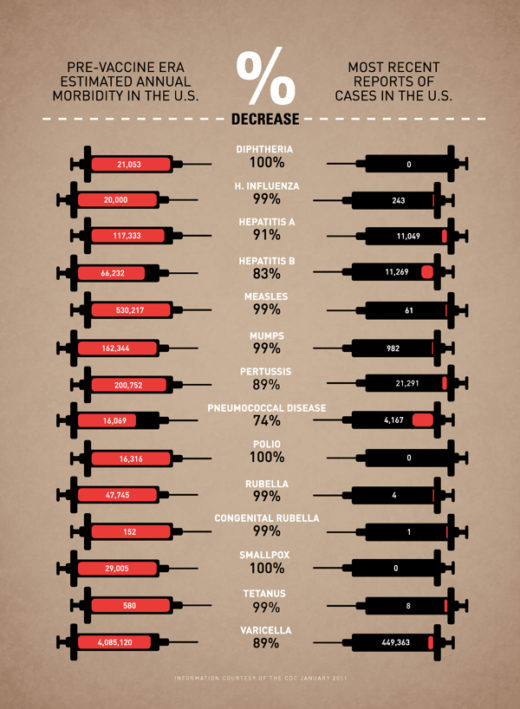
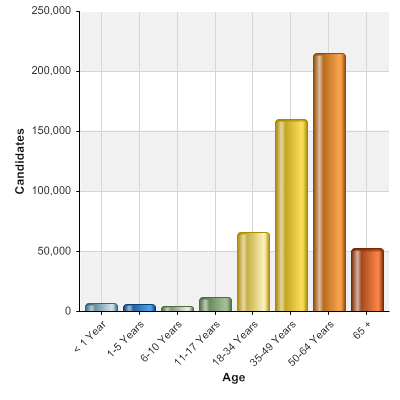
The scientific evidence that vaccines work is indisputable, and as the below infographic summarizes, their impact on morbidity from communicable diseases is miraculous. Sadly, now that the anti-vaccine movement has streamlined into the general population, anxious parents are conflicted as to whether vaccinating is the right choice for their children. We must start by going back to the basics of what a vaccine actually is and how it works. Next, we must reiterate the critical importance that maintaining herd immunity above 92-95% plays in protecting not only those too young or immunocompromised to be vaccinated, but even fully vaccinated populations. If all else fails, try emailing skeptical friends and family a clever graphic cartoon that breaks down digestible vaccine facts. Simply put: getting vaccinated is not a personal choice, it’s a selfish and dangerous choice.
The Panic Virus is first and foremost an incredibly entertaining, well-written narrative of the dawn of an anti-vaccine phenomenon which has reached a critical mass. It is also an important case study and cautionary tale about how we process and disseminate information in the age of the Internet and access to instant information. It is also an indictment on a trigger-happy, ratings-driven, sensationalist media that reports “news” as they interpret it first, and bother to check for facts later. In the case of the anti-vaccine movement of the last few years, the media fueled the fire that Andrew Wakefield started, and once a gaggle of angry, sympathetic parents was released, it was difficult (if-near impossible) to undo the damage. This type of journalism, Mnookin writes, “gives credence to the belief that we can intuit our way through all the various decisions we need to make in our lives and it validates the notion that our feelings are a more reliable barometer of reality than the facts.” Sadly, the autism-vaccine panic movement is not an outlying incident, but rather a disconcerting emblem of a growing anti-science agenda. The UN just released its most dire and alarming report ever issued on man-made climate change impacts, warning that temperature changes and industrial pollution will affect not just the environment, extreme weather events and coastal cities, but even the stability of our global economy itself. Immediate rebuttals from an influential lobbying group tried to undermine the majority of the scientists’ findings. So toxic is the corporate and political resistance to any kind of mitigating action, that some feel we need a technological or political miracle to stave off a certain environmental crisis. At a time when physicists are serious debate on evolution versus creationism and thousands of public schools across the United States use taxpayer funds to teach creationism in the classroom.
Mnookin’s book is an important resource and conversation starter for scientists, researchers and frustrated physicians as they carve out talking points and communication strategies to establish a dialogue with the public at large. When young parents have questions about vaccines (no matter how erroneous or ill-informed), pediatricians should already have materials for engaging in a positive, thoughtful discussion with them. When scientists and researchers encounter anti-science proclivities or subversive efforts to undermine their advocacy for a pressing issue, they should be armed with powerful, articulate communicators — ready and willing to deliberate in the media and convey factual information in an accessible way. When Jenny McCarthy and a gaggle of new-age holistic herbologists were peddling their “mommy instincts” and conspiracy theories against vaccines, far too many scientists and physicians simply thought it was beneath them to even engage in a discussion about something whose certainty and proof of concept was beyond reproach. Now, the newest polling suggests that nothing will change an anti-vaxxer’s mind, not even factual reasoning. Going forward, regardless of the issue at hand, this type of response can never happen again. The cost of complacency or arrogance is nothing short of life or death.
The Panic Virus by Seth Mnookin is currently available on paperback and Kindle wherever books are sold. For further reading on how to deal with the complexities of the anti-vaccine movement aftermath, we suggest the recent book On Immunity: An Inoculation by Northwestern University lecturer Eula Bliss.
*****************
ScriptPhD.com covers science and technology in entertainment, media and advertising. Hire our consulting company for creative content development. Follow us on Twitter and Facebook. Subscribe to our podcast on SoundCloud or iTunes.
A Father’s Love and a Scientist’s Dedication in a Race against Time
Imagine this scenario: you are a young married professional, a rising star in a well-respected pharmaceutical company. You have three children, two of which suffer from a rare, inherited genetic disease for which there is no cure. They will die in about a year or two. What do you do? Inspired by the book The Cure: How a Father Raised $100 Million – and Bucked the Medical Establishment – In a Quest to Save His Children by Pulitzer Prize-winning journalist Geeta Anand, Extraordinary Measures is a drama about the real-life story of John Crowley (Brendan Fraser) and Dr. Robert Stonehill (Harrison Ford) as they work feverishly to find a cure for the disease afflicting Crowley’s children. The dramatic caveat is that said cure is based solely on a scientific theory. CBS Films’ motion picture debut touches on a myriad of salient modern-day issues, including personal morality, risk taking, scientific funding, pharmaceutical business practices, the dedication to science, professional relationships, and a man’s love for his family. For the full ScriptPhD.com review, please click “continue reading”.
REVIEW: Extraordinary Measures
ScriptPhD Grade: B+
Extraordinary Measures opens with an ambitious John Crowley (Brendan Fraser) rising up the corporate ladder in the global biopharmaceutical company Bristol-Myers Squibb. Despite two of his three children having a rare genetic disorder called Pompe Disease (pronounced Pom-pay). The family lives a relatively normal life, where birthday parties are celebrated and the children remain upbeat despite their condition. By day Mr. Crowley is a businessman, husband and father, by night he is lunging himself into the daunting world of reading scientific journals in the field of biochemistry, attempting to find and contact any scientist he feels may be on track to developing a cure for his two children. Throughout all of his heroic efforts, he is faithfully supported by his wife Aileen Crowley (Keri Russell).
During one Mr. Crowley’s many nights of pouring through scientific papers, he comes across the research of Robert Stonehill, MD, PhD. Dr. Stonehill is a role based on the real-life glycobiologist Dr. William Canfield. What is glycobiology and how does that involve Pompe disease? A glycobiologist is a scientist who studies sugars, and the enzymes which add sugar molecules to proteins. It is these enzymatic chemical modifications where Dr. Canfield is a leading expert and researcher. Pompe Disease is a rare (estimated at 1 in every 40,000 births), inherited and often fatal disorder that disables the heart and muscles (excellent overview). It is caused by mutations in a gene that makes an enzyme called alpha-glucosidase (GAA). Normally, the body uses GAA to break down glycogen, a stored form of sugar used for energy, in muscle cells. But in Pompe Disease, mutations in the GAA gene reduce or completely eliminate this essential enzyme. Excessive amounts of glycogen accumulate everywhere in the body, but the cells of the heart and skeletal muscles are the most seriously affected. Researchers have identified up to 70 different mutations in the GAA gene that cause the symptoms of Pompe disease, which can vary widely in terms of age of onset and severity. The severity of the disease and the age of onset are related to the degree of enzyme deficiency. If a person has only one mutated form of this gene and one normal copy, they are only a “carrier”—that is, they can pass it down to their children, but they themselves do not develop the disease. A person needs to have both copies of the mutated gene in order to have the disease. The Crowley children inherited the mutations for this disease from each parent.
The movie portrays Dr. Stonehill as a brilliant, albeit eccentric, scientist as dedicated to the pursuit of science as he is a cure, and Mr. Crowley as a devoted, loving father who will not quit in his search for a cure. Convinced Dr. Stonehill is on the right track to producing a therapy for Pompe disease, Mr. Crowley is able to meet Dr. Stonehill, currently working as a scientist at a university. Dr. Stonehill, while brilliant and confident in his scientific research and theories, admits that ultimately his work is only theoretical, and not yet empirically proven. Mr. Crowley asks Dr. Stonehill what would it take to get his research from the bench to the bedside of his children and others like them. In short, and bitterly reflective of modern pharmaceutical realities, Dr. Stonehill replies “money.” Dr. Stonehill informs Mr. Crowley that not all sound theories in science are funded, the competition for grant money is fierce. In addition, while Dr. Stonehill loves his research he is frustrated by the university owning the patent rights to his ideas. At this point, Mr. Crowley informs Dr. Stonehill there is a Pompe Disease Foundation which will fund his research. They agree to meet again later in time.

During this time, Mr. Crowley, who is still working for Bristol Myers Squibb, begins to realize his continued employment with the pharmaceutical behemoth might forever endanger finding a cure for his children. Concurrently, he and his wife struggle with the quandary of letting nature take its course versus the moral/ethical implications of trying to fix their children’s condition. Should Mr. Crowley quit his good-paying position, and leave to pursue a cure? Mr. Crowley and Dr. Stonehill decide to start a business together, seek out venture capitalists and ultimately receive the funds necessary to start a small biotechnology company. The issues (and there are many!) of starting and running a biotech company, something neither of them has ever done, are adroitly explored throughout the movie. When investors realize the company is burning through millions of dollars, they give Crowley and Stonehill an ultimatum: merge with someone who can make this drug or we are turning out the lights for good.
The company they form, Priozyme (the actual erstwhile Novazyme), is eventually bought by the fictitious pharma giant called Zymagen. In real life, Zymagen was actually the biotech company Genzyme. Zymagen already has three Pompe research teams, which Dr. Stonehill arrogantly believes this is because they don’t really know what they are doing. Dr. Stonehill is made the chief scientist for what is now Zymagen’s 4th Pompe research team. Mr. Crowley is made the Senior Vice President for the Pompe project, much to the dismay of Zymagen scientists, due to his lack of scientific training. Extraordinary Measures does a good job of portraying the acquisition as a clash between personalities (which is rampant in science) and the often-embraced adage in the scientific community that non-scientists cannot contribute to or advance scientific research to a measurable degree. In addition to Dr. Stonehill’s personality not being received well by Zymagen, Mr. Crowley has his own problems with their corporate leadership. At Zymagen each Pompe disease research team works on its own. The teams do not collaborate with each other at all, with no sharing of information. The corporate leadership believes this brings out the best; Mr. Crowley believes this significantly slows down scientific progress.
Ultimately, although Dr. Stonehill’s candidate enzyme is selected for clinical trials, a bevy of ethical concerns and scientific roadblocks stand in the way of getting the discovery past the laboratory and on the way to FDA approval. Mr. Crowley, who selflessly gave up virtually everything towards the discovery of a Pompe cure, must make the ultimate sacrifice in order to ensure that it is able to help his children. Incidentally, on April 28, 2006 the Food and Drug Administration granted marketing approval for Myozyme® (alglucosidase alfa) in the U.S., indicated for use in patients with Pompe disease (GAA deficiency). While Extraordinary Measures doesn’t get into the gritty details of the true politics behind a lot of pharmaceutical company drug target choices, funding and scientific arm-wrestling, it does an excellent job of giving the lay public a general overview, which has been (with the exception of the brilliant The Constant Gardner) largely cinematically absent. For anyone curious about the drug discovery process, and the anguish both on the part of families and scientists desperately hoping for a cure, this movie is a must-see.
Brendan Fraser on playing the real John Crowley: click here.

Extraordinary Measures goes into wide release on January 22, 2009 in theatres nationwide
Trailer:
NeuroScribe obtained a BS in Biology, and a PhD in Cell Biology with a strong emphasis in Neuroscience. When he’s not busy freelancing for ScriptPhD.com he is out in the field perfecting his photography, reading science policy, and throwing some Frisbee.
~*NeuroScribe*~
*****************
ScriptPhD.com covers science and technology in entertainment, media and advertising. Hire our consulting company for creative content development.
Follow us on Twitter and our Facebook fan page. Subscribe to free email notifications of new posts on our home page.
]]>
Medical shows are a generational television staple—often dramatic, rarely realistic, and only sometimes socially relevant. But tonight, on CBS, a different kind of medical show premiered. Three Rivers, based at a fictional world-famous transplant hospital in Pittsburgh, puts front and center an often misunderstood and ignored sector of modern medicine—organ transplantation. With wit, sensitivity, and a refreshing degree of accuracy, this important new show will shed light on the three branches of the organ donation and transplantation system: the donors, the recipients, and the transplant surgeons and staff who connect the two. Under the jump, ScriptPhD.com reviews the pilot and provides important information and resources for those who are considering signing up to be a donor.
Review: “Three Rivers” (CBS)
The characters and setup will seem familiar to anyone who watches medical shows on a regular basis. There is Dr. Andy Yablonski, the dashing, brilliant, yet arrogant surgeon who is too busy saving lives to be concerned with the boring details of being a doctor (Alex O’Loughlin). Dr. Miranda Foster (Katherine Moening) is as damaged as she is earnest, and lives and dies with each patient she will save. The hospital’s shiny new transplant coordinator Ryan Abbott (Christopher Hanke) is learning the details of transplantation on the job, and so is the audience along with him (nice touch!). Tethering this crew is the matronly, austere hospital administrator Dr. Sophia Jordan (Alfre Woodard). Unfamiliar, and exposed on television for the first time, is the tense pressure-cooker setting in which these doctors perform their job: a nationally renowned transplant center, Three Rivers Hospital. The organs are what interconnect seemingly discordant lives—a workplace accident in Cleveland, a pregnant patient experiencing heart failure in Pittsburgh and an African who traveled the world in search of the best transplant care—and the heroic doctors, and generous families are what make it all possible. Medical shows have certainly broached organ transplantation before, but Three Rivers takes it one step further to present a real-time tapestry of the complex players and paths that must come together to pull off what is quite an impressive feat. The show is fast-paced, innovative, and written cleverly enough to allow forgiveness of divergence into occasional tired cliché territory.
What they got right…
A lot, actually. The devil’s in the details (especially in television dialogue), and Three Rivers surprises and delights with how many they expertly weaved in to the overarching storylines. Some were throwaway, yet crucial—Dr. Yablonski using Purell on his hands before touching a (likely immunocompromised) patient. Also noteworthy were certain facts, myths and misconceptions about donation sprinkled in throughout the pilot (103,000 patients currently on the waiting list). The Three Rivers writing staff just needs to mind that they continue to incorporate them into the storylines, lest they risk sounding overly preachy or didactic. Others were more overt, such as how quickly difficult decisions must be made when an organ is at stake. The husband who must decide on a C-section versus a transplant for his wife would indeed have only hours, maximum, to make the choice before transplant doctors moved on to the next patient on the waiting list. Finally, and most importantly to the show’s greater thematic ambitions, Three Rivers provides a delicate balance to not undermining the tragedy of the victims (donors) in exchange for celebrating the lives they will eventually save (the recipients).
Missteps…
My two biggest problems with the pilot were in the hospital presentation and rosy picture of organ availability and mobility. I don’t know how often the writers of this show have visited hospitals in the United States, even the modern, new ones, but they don’t look remotely like the fictional “Three Rivers”. Surrounded by glass and neo-modern angular architecture, this hospital spares no expenses in the technology department: magical touch-screens in every conference room, three-dimensional mobile radiology lab results, and 1,000 channels in every patient’s room. Someone needs to tell President Obama about this wizardry; it could really change the universal health care debate in this country! Secondly, the show takes some loose liberties with how quick of a turnaround transplant patients can expect when they walk into a hospital, and which patients can expect to get organs. Dr. Yablonski grins as he promises his African patient a new heart, despite no insurance coverage and magically procures a heart at will for a pregnant patient. The truth is that all the good intentions in the world can’t supersede or bypass the strict, immutable guidelines established by the United Network for Organ Sharing, the official arbiter of the nation’s organ waiting list that facilitates every organ transplant performed in the United States. Yes, the wealthy, the connected, and special snowflakes like Steve Jobs can often massage the system to bypass spots on the national queue, something that has stirred passionate debate about the true equity of the system, but by and large, a patient’s spot on the list, and their mobility within it, is determined by factors such as direness of illness, length of wait, and, yes, regional location. Unfortunately, even in the most critical circumstances, the sickest patients die every day waiting for an available organ, another great reason to become a donor today (see below). It is my hope that, while uncomfortable, future episodes will address this sad reality.
Despite these minor quibbles, the ScriptPhD is delighted to see a television show entertain, educate, and strive to embed consciousness towards, and give a compassionate face to, organ donation. It is highly likely that this television show will save thousands of lives simply by telling these stories and motivating viewers to become donors and talk about it with their extended families and friends, and that is a priceless dividend for art transcending life.
Three Rivers airs on Sundays at 9 PM ET/PST on CBS.
The Gift of Life
In an unusual degree of social outreach for a television show, CBS and Three Rivers are partnering with Donate Life America, an educational vehicle of the medical transplant community established in 1992. “We have been working with Donate Life to ensure ‘Three Rivers’ accuracy,” said executive producer/creator Carol Barbee. “We are hoping that the awareness from our show and the outreach from the combined efforts of CBS and Donate Life will result in an increase in donor registration which in turn will save lives.” In addition to council on technical aspects of the show’s content, a widespread organ donor awareness campaign by CBS will include green donor bracelets and literature at various studio properties to live audiences, a donation campaign at DMV locations throughout the country, and special public service announcements involving stars from the show. Donate Life is actively involved in digital social media outreach, and you can follow them on their Facebook page and various Twitter discussions (#DonateLife).
Currently, over 103,977 men, women and children await life-saving organ transplants (as of October 1, 2009). Complicating the efforts of physicians, health care providers and transplant organizations to raise awareness and giving are misconceptions and outright fallacies about the donation process, patient qualifications and religious and moral considerations to donation. Some of these include:
Financial cost: There is no financial cost associated with becoming an organ donor. If you are a recipient, there are several common funding sources for financing a transplant that may be found here.
Religious objection: All major religions either accept organ donation or the right of the individual to choose to donate. If you are conflicted, talk to your clergymember about the issues involved and set your mind and heart at ease that the important decision you are making falls in line with your spiritual and religious views and obligations.
Age restrictions: There are none. The only qualification on organ donation (living or deceased) is health, not age. If you sign up to be an organ donor, the transplant doctors will decide whether you qualify. Qualifications for living donors may be found here.
Signing up is complicated: Quite the opposite. In most cases, it’s as easy as signing a donor card, DMV permission form, or finding out how to be a living donor through the United Network for Organ Sharing.
And this is a big one…
Doctors will not try as hard to save the life of an organ donor: This commonly propagated piece of misinformation is simply NOT TRUE. Doctors who treat patients at the time of illness or death are not involved in either obtaining consent for organ donation or the transplantation itself (this is handled by a different team of surgeons). As such, every effort is made to save the life of every patient, regardless of donor status.
To help address some of the topics we’ve broached, and provide many more detailed answers for potential donors, recipients and their loved ones, please visit some of these important organ (and blood and bone marrow) donation agencies and organizations:
•United Network for Organ Sharing (UNOS), the official transplant recipient waiting list organization
•Donate Life America
•OrganDonor.gov, the official U.S. Government page on organ donation and awareness facts
•Transplant Living, the official resource page for transplant patients and living transplant donors (non-deceased donors).
•American Society of Transplantation, the research and medical professional association of transplant specialists.
•My Angel Foundation, providing support and inspiration to recipients and donors, as well as their families.
•National Bone Marrow Registry Are you registered to be a bone marrow donor? It’s easy, relatively risk-free, and you could save a life today.
•GiveLife.org Find a blood drive near
you through your local Red Cross.
To find out how to become an organ donor, click on your state for detailed information. Simply marking “yes” on your driver’s license is not enough in some cases to be considered a donor. You can also download and sign organ donor cards to carry with you in your wallet.
Ultimately, the decision to become an organ donor can be summed up with a poignant line from the Three Rivers pilot: “It has to be a gift.” It is one of the most personal, heart-wrenching, difficult decisions an individual can make, and one that is often asked of families under pressured, stressful, confusing circumstances. But this does not have to be so. Have those discussions with your loved ones and make your wishes clearly known now. And if you need some added inspiration about how much the gift of life can live on in those that receive transplants and make a difference to the families of those that give, check out some of these inspiring stories and a video of a heart transplant recipient’s letter to her donor. ScriptPhD.com humbly asks you to please peruse the links we have provided to consider if organ donation—the gift of life—might be the right decision for you and your family.
~*ScriptPhD*~
*****************
Follow ScriptPhD.com on Twitter and our Facebook page. Subscribe to email alerts for new posts on our home page.

ScriptPhD.com recently reviewed and recommended a new medical mystery thriller, “Beat the Reaper”, written by real-life medical doctor Josh Bazell. A longtime aspiring writer, Josh majored in English Literature with Honors at Brown University, after which he entered the English Lit PhD program at Duke. He ultimately chose to pursue a post-graduate degree in medicine at Columbia University, and completed his residency in the Department of Psychiatry at the University of California at San Francisco. He is currently working on his second book and is a practicing psychiatrist.
In between getting ready to release “Beat the Reaper” as a paperback, with a Leonardo di Caprio-starring film adaptation in the works, and writing his follow-up novel, a busy Dr. Bazell generously lent us some time to chat. To read our interview, please click “continue reading”.
ScriptPhD: Josh, your trajectory into medicine was very unique. You really epitomize our site’s embrace of the interface between science and the arts. You were an English major at Brown University, and you actually optioned a screenplay before going on to medical school at Columbia. Did you always have the dual interest? What ultimately tore you away from exclusively writing and towards medicine?
Josh Bazell: I started out writing fairly young, then worked in a cognitive neuroscience lab in high school and got into science. I put off medical school as long as I could because I worried it would take too much time away from writing, but eventually I got so old I had to either go or not, which clarified things.
SPhD: I was curious where the idea for “Beat the Reaper” first entered the fray. I’m assuming (and hoping!) it didn’t come from any personal experience with the Mob.
JB: Prior to researching Beat the Reaper my experience with the Mob was more or less what anyone’s would have been growing up near Sullivan Street in lower Manhattan: I saw a lot of guys who wanted people to think they were dangerous, and some of them probably were. My real interest, though, like most people’s, probably comes from The Godfather.
SPhD: I couldn’t put the book down in the two days it took me to read it. For me, above all, Pietro Brnwa’s character decidedly drove that momentum, and my sympathy and concern for him fed into the overall suspense that builds throughout. For many reasons that we’ve discussed in the above review, he defies mafia stereotypes. He has a moral code, he follows it, and underneath that gruff, snarky exterior, one could almost say he’s really very sweet and cares. Did you set out to write a character like this at the beginning of the process and do you mind sharing your perspective of Pietro and his motivations?
JB: Yeah, the idea was for Pietro to be someone you couldn’t help liking even though you might not want to. A lot of his actions are inexcusable, but it’s hard, for me at least, not to sympathize with someone who’s gone too far off the rails to ever get back but nonetheless feels compelled to try. What people make of their fucked up lives is always more interesting to me than how they turn out if everything goes well.
SPhD: At the end of the book, without spoiling the specific ending, Pietro has a choice to make between surefire escape to safety from the hit men tailing him and going back to the hospital, because he’s just figured out a way to save a patient’s needless leg amputation. He chooses the medicine, chooses to solve the puzzle, and to declare it his destiny, which also sets up the denouement quite nicely. It’s a little symbolic of the choices you had as your writing career ascended, but you also went to med school and back into the hospital after the book came out and continued your medical practice. Do you feel like medicine is your destiny and can you talk a bit about choosing psychiatry as a specialty?
JB: There’s definitely some of that tension, if not ambivalence, in my life. The book actually sold early in my second year of residency, at which time I had patients and a contract. When the year ended I took a leave of absence to write the next one. I would like to keep both things in my life if I possibly can, and am still figuring out how to make that happen. As to why I chose to go into psychiatry: to paraphrase Willie Sutton, that’s where the pain is.
SPhD: The style of your writing reminded me a LOT of Ernest Hemingway, particularly the realistic, declarative dialogue (an ode to your screenwriting background, perhaps) and Pietro’s wry, colloquial, natural storytelling voice. And I say this as a compliment, since Hemingway is my favorite American author. Who do you enjoy reading and would you say influenced your writing style the most?
JB: Thanks. I like Hemingway a lot, and see him as essential to the morally exhausted tough-guy voice that evolved around the time of The Sun Also Rises. I’ll read anything that feels energetic and honest. My background is in classics and crime fiction (I’ve got a full reading list coming out at the back of Beat the Reaper), but these days I’m mostly reading non-fiction. To me it’s about trying to make sure that one’s writing takes place in the world rather than in some alternate reality that we know (to death) from movies and books. I think sounding like Hemingway does now is infinitely easier than sounding as exciting as he did in 1926. But that’s always the goal, and I’m always looking for it in other people’s work as well.
SPhD: You wrote “Beat the Reaper” during your internship in your “spare time”. The internship is the first year of residency, otherwise known as Hell on Earth. I have a doctor friend who didn’t even have time to do laundry; she just bought new clothes. How did you allocate time to write a stupendous medical thriller?
JB: I really like writing, so it felt recreational rather than something I had to make time for. Like your friend, I didn’t do much laundry either. I still don’t, sometimes.
SPhD: Can you share a little sneak peak of your current project with ScriptPhD.com? Any chance that we’ll see our good friend Bearclaw again?
JB: I’m writing another book about him now. Whether it will see the light of day remains to be seen.
SPhD: Thanks so much for your time, Josh! We wish you all the very best in the future!
JB: Thanks very much for your interest.
~*ScriptPhD*~
***************
Follow us on Twitter and our Facebook page.
Beat the Reaper: A Novel
Written by: Josh Bazell
House meets The Sopranos—there’s your Hollywood pitch line for the debut novel of talented newcomer Josh Bazell. But it’s so much more than that: part medical mystery, part action-adventure thriller, part character study, Beat the Reaper deftly explores the scope of revenge, loyalty and one’s capacity for redemption. We are introduced to the novel’s protagonist, a New York City doctor, as he’s getting mugged on his way to work. But rather than acquiescing, he expertly dislocates the mugger’s arm, smashes his nose in and takes his gun. Peter Brown is clearly no ordinary doctor. Left to fend for himself at the age of 14 after the vicious murder of his grandparents, Pietro Brnwa takes up karate and a fateful friendship with David Locano, aka Skinflick, whose father was a lawyer by day, a mobster by night. Initially attracted to the mafia for personal retribution, Brnwa descends deeper into the Locano family and their ties, and finds that he is disturbingly good at his job. A perfectly orchestrated series of events leads Pietro into murder, a test of his friendship with Skinflick and the threat of jail. Instead, he ends up at dingy, dilapidated Manhattan Catholic Hospital as Dr. Peter Brown, a member of WITSEC, the U.S. Marshal’s Service Witness Security Program. Peter’s anonymity comes to a crashing halt when he treats a blast from the past, in the form of terminally ill patient Eddy Squillante, who recognizes him as the erstwhile “Bearclaw” Brnwa. As long as he can keep Squillante alive, he staves off some angry mobsters looking to get reacquainted. To do so, he must navigate through a sea of other patients, a shady surgeon assigned to Squillante’s case, and external forces looking to ensure that he fails. Oh and by the way, he has eight hours. (Why is Peter known to the mobsters as Bearclaw? You’ll have to read the book and find out… it’s downright incriminating!)
Pietro Brnwa is a unique, memorable character in the best tradition of detective fiction heroes. Not one you’d call warm and fuzzy, he ascribes himself as “God’s original asshole” and his sycophantic medical students as “two cups of human misery in short white coats”. He has a short temper, a snarky aside for most everything and everyone that crosses his path, and generally looks at the glass as half empty. But Pietro also has a defined moral code of ethics. His very reason for joining the Mafia—to avenge his grandparents’ senseless death—is practical, not glamorous. He won’t kill women or children, as evidenced by his refusal to kill the sister of the man that sold his grandparents to Auschwitz. And he manages to show a tender side with the only woman he’s ever loved, and who plays a tragic role in the final showdown between his past and present. More importantly, Brnwa, as Peter Brown, is an excellent doctor. Sure he has plenty of insults for fellow physicians, no patience for patients, and crunches on Moxfane tables to stay awake enough for rounds. But he also cares enough to make time for a frightened cancer patient awaiting surgery, to retrieve a lost well-meaning elderly patient with dementia and to perform an impossible surgery on the dying Mob messenger that’s been sent to warn him. Okay, that last one was a necessity.
On top of the intricate action, mind-bending medicine and humor, the book’s style is immensely enjoyable—sexy, sleek, fast-paced, and a little too cool for old school. Bazell unfolds the plot cleverly with side-by-side storylines. Peter Brown’s impending peril is told compactly over the course of the eight hours that interweaves his reunion with old friends with an interesting medical mystery and a rather unfortunate incident with an Assman and a needle. All in a day’s work. Concomitantly, Pietro Brnwa’s story transpires over a more protracted period of time, and the reader absorbs the tragedies that befell Pietro from his early days in the mob through to the deal that lands him in witness protection, learning what makes him tick along the way. The past merges seamlessly with the present to culminate in an ending so shocking and imaginative, you will want to have an anatomy textbook, not to mention a strong stomach, to piece it all together. Interspersed throughout are little factoids and medical footnotes that add a rich third dimension to the novel’s flow and to our protagonist’s hilariously sarcastic wit. Did you know that scrub suits are reversible, that some of the most prosperous pharmaceutical companies had a shameful history of slave labor at Auschwitz, that you can’t run DNA tests from urine, that surgeons will use some pretty superfluous silly vocabulary to avoid saying “head up” or “head down” in surgery, or the real reason that Tony Soprano’s cover as a garbage consultant is ironic? Neither did I. Rarely does a thriller afford you the opportunity to pick up some knowledge while you’re being entertained, and for that, Beat the Reaper gets the ScriptPhD.com seal of approval!
As if all of this isn’t enough to get you excited, the book is currently being adapted for film by the same team of screenwriters that brought you Ocean’s Thirteen. There are even rumblings of Leonardo DiCaprio playing Peter Brown/Pietro Brnwa/Bearclaw. So go out and please support a local bookstore in picking up a copy today!
~*ScriptPhD*~
]]>Suddenly, in the world of TV medicine, RN are the letters you want after your name. Two summer cable shows garnering considerable buzz, SHOWTIME’s Nurse Jackie and TNT’s HawthoRNe, shine the spotlight on nurses, the hospital heroes often relegated into the shadows of doctors on prime time. ScriptPhD.com got a sneak peak of the HawthoRNe pilot and the first half of the Nurse Jackie season.
Nurse Jackie (SHOWTIME)
ScriptPhD Grade: A
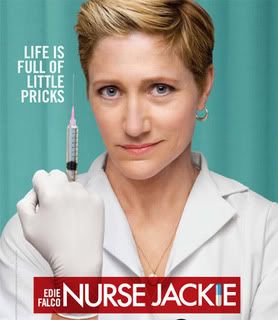
I didn’t want to love Nurse Jackie, I just want to say that for the record. First of all, she’s been taunting me on the billboards of Los Angeles all spring and summer long with that intimidating needle. Secondly, I didn’t know if I had it in me to get attached to yet another medical show. Third, after hooking me with brilliant shows like Dexter, Weeds and newcomer The United States of Tara, could SHOWTIME extend their magic touch to this newest addition to their franchise? They could, they did, and the result is some of the freshest television this side of basic cable. Starring three-time Emmy®-winner Edie Falco, Nurse Jackie is based on the provocative tell-all journal of a real-life Manhattan nurse. Shot on location in New York City, the show spares nothing in projecting the goings-on of a big-city ER through the eyes of one very unorthodox nurse.
And Jackie Peyton is certainly not an easy character to love. She’s decidedly cantankerous and has little time for people or their stupidities. “I don’t do chatty,” she barks. “I like quiet. Quiet and mean. Those are my people.” She’s got an unhealthy attachment to painkillers. No matter the delivery system (mouth, nose, coffee) or the type (Adderall, Vicodin, OxyContin, Percocet), Jackie’s not very picky. She views rules as bendable at best, nonexistent at worst. Oh yeah, and then there’s the part where she’s cheating on her husband. But there’s two sides to every coin, and Jackie is no exception. At home, he’s a devoted wife and mother. Her picture-perfect husband Kevin (Dominic Fumusa) struggles between tending to their daughters Grace, sporting an escalating emotional anxiety disorder, and Fiona (Ruby Jerins and Daisy Tahan) and running his bar. At the ironically named All-Saints Hospital, she’s an extraordinary, deeply empathetic nurse. Whether she’s helping a 10-year-old take care of her mom with some contraband pharmacy supplies, assisting a terminally ill fellow nurse, helping a mute stroke victim shut up his obnoxious family or stealing money from a criminal to help a dead patient’s poor fiance, Jackie weaves through the murky moral grey area to ultimately do what’s right for her patients. Part saint, part sinner, Nurse Jackie is never less than totally compelling.
Trailing Jackie’s every move (much to her dismay) is overly earnest, perky nursing student Zoey Barkow (Merritt Weaver). Luckily, Jackie can take reprieve from her besotted young acolyte and her problems with the rest of her hospital family. Providing cover is her partner in crime, fellow nurse Mohammed “Mo-Mo” de la Cruz (Haaz Sleiman), with whom she bends the rules, shares coffee breaks and romantic advice. Providing narcotics and lunchtime quickies is pharmacist Eddie Walzer (Paul Schulze). Her best friend and confidante is the wry Brit Dr. Eleanor O’Hara (a razor-sharp Eve Best). She has a penchant for expensive clothes, snappy comebacks and mid-town lunchcapades with “Jacks”, but seems to be holding back a painful past. Peter Facinelli (Damages) is the handsome, young Dr. Fitch “Coop” Cooper, who could easily be dismissed as a one-dimensional, book smart but inept playboy. But with lesbian moms (the devine Blythe Danner and Swoozie Kurtz), a proclivity for Tourette’s-like inappropriate touching, and better doctor skills than he gives himself credit for, Coop is more than meets the eye. Rounding out the ensemle is rote ER administrator Gloria Akalitus (The West Wing’s Anna Deveare Smith), who rules with an iron fist, thinking she’s hip to every trick in the book. (By the way, who knew Deveare Smith had such a gift for physical comedy? Two gags with a Taser and some wayward painkillers had me rolling on the floor.)
Employing top-notch writing and directing, led by creative team Evan Dunsky, Liz Brixius and Linda Wallem, Nurse Jackie shies away from tired old medical show tropes to peel back the layers of a functional addict leading compartmentalized lives, to realistically show the challenges nurses face in saving lives under the limitations of our broken medical system, and to ask, “What does it really mean to be good?” Nurse Jackie may be addicted to bad behavior and every painkiller on the planet, but in the end, I’m addicted to her. I wouldn’t have it any other way.
Nurse Jackie airs on SHOWTIME Mondays at 10:30 EST/PT, following Weeds.
HawthoRNe (TNT)
ScriptPhD Grade: B

A number of high-profile film actors have recently settled comfortably in starring TV roles, most successfully Emmy® winners Glenn Close (Damages) and Alec Baldwin (30 Rock). TNT, with their long and storied tradition of strong female drama leads, from Kyra Sedgwick’s The Closer to Holly Hunter’s Saving Grace, extends the same small-screen opportunity to Jada Pinkett Smith, who stars in new medical drama HawthoRNe. Lest there be any doubt about the girl power behind this series, it is being co-produced by Pinkett Smith’s 100% Womon [sic] Productions. In the first five minutes alone, Christina Hawthorne races to Richmond Trinity Hospital in the middle of the night, out(wo)mans an armed security guard, tends to a wandering psych ward patient, pays care to a homeless woman she’s befriended and talks down a suicidal cancer patient. But it turns out, there are some cracks in Christina’s impenetrable armor. For one, the pilot takes place on the one-year anniversary of the death of her husband, whose ashes she still talks to. To celebrate, her rebellious, headstrong daughter Camille (Hannah Hodson) chains herself to the school’s vending machine, much to her mother’s consternation. And a deliciously saccharine Joanna Cassidy is the still-meddling mother-in-law who also serves on Trinity’s board.
As the hospitals Chief Nursing Officer, Christina is organized, uncompromising, decisive, empathetic, and always puts the needs of patients first. Her charges include nurse Bobbie Jackson (Suleka Matthew), one of her best friends and nurse Ray Stein (David Julian Hirsh), a man caught in a woman’s world. Alias’s Michael Vartan (welcome back to television Mr. Vaughn!) is Dr. Tom Wakefield, the Chief of Surgery with whom Christina often butts heads administratively, but who also treated her late husband for cancer.
Still working out its kinks, HawthoRNe feels a bit uneven at times, mostly due to relying on some trite, atavistic medical formulas that come off stale. A genuinely compelling storyline about a homeless woman besieged with mental problems giving birth outside the hospital is negated by an unnecessary (and gross!) side plot involving a grateful nurse (Christina Moore)…um…thanking a wounded soldier for his service. Her name is Candy. Seriously. And a chance to explore doctor-nurse synergy and conflict in providing effective patient care turns downright silly when the characters in question ride two extremes: the stupendously arrogant, omniscient doctor whose decisions Cannot. Be. Questioned. and the equally timorous nurse who dare not think independently. And don’t forget to save some snickers, because he’s a male nurse, which is funny, or was in 1975.
TNT may know drama, but HawthoRNe needs to tone it down a bit. To be fair, having only viewed the pilot, the show has definite potential to grow. With the departure of ER, no current medical show centerpieces medicine in a cash-strapped, blue-collar city hospital. Set in Richmond, VA, HawthoRNe has a unique opportunity to tell stories pertaining to the challenges of its setting and patient population. It also is clearly a character-driven drama, establishing some fascinating early relationships. The tension between Christina and her bitchy mother-in-law, tempered by working through the shared grief with her still-angry daughter, makes for a rather interesting family triangle. And sparks fly between Pinkett Smith and Vartan, who is obviously being set up as a potential love interest. But the biggest asset is Pinket Smith herself. She brings an intensity, compassion and resolve to a complex character. Her movie star power translates well to the small screen, and could easily make HawthoRNe a fine vehicle for her considerable acting chops. Assuming they steer clear of Clicheland.
HawthoRNe premieres this Tuesday, June 16th on TNT at 9 EST/PT.
This sudden focus on the nursing profession doesn’t come a minute too soon. According to the American Association of Colleges of Nursing, the United States is in the midst of an imminent nursing shortage, compounded by the rapidly aging baby boomer population and low enrollment in nursing programs that is not expected to meet this demand. As of July, 2007, total RN vacancies across the US totaled 135,000, or 8.1%, according to a report released by the American Hospital Association. Projections from the U.S. Bureau of Labor Statistics published in the November 2007 Monthly Labor Review foresee that more than one million new and replacement nurses will be needed by 2016. Contributing factors vary, from a shortage of nursing school faculty and projected enrollments, to a slowing rate of growth for the overall nursing population, resulting in a climbing average age of the nursing population. The result for nurses? Insufficient staffing is raising their stress levels, impacting job satisfaction, and driving many nurses to leave the profession. The result for patients? Inadequate access to quality health care. An eye-opening report released in August 2002 by the Joint Commission on Accreditation of Healthcare Organizations, revealed that a shortage of nurses in America’s hospitals is putting patient lives in danger. JCAHO examined 1609 hospital reports of patient deaths and injuries since 1996 and found that low nursing staff levels were a contributing factor in 24% of the cases.
Less than a month ago, members of major nursing unions that included the California Nurses Association/National Nurses Organizing Committee, the United American Nurses (UAN), and the Massachusetts Nurses Association, congregated on Capitol Hill as part of a National RN Day of Action in Washington, D.C., that included a conference focused on promoting legislation that would guarantee certain ratios of nurses to patients nationally, a march and rally, and visits to their congressional representatives to advocate on various legislative issues. The legislation, House Resolution 2273, also seeks to protect the rights of nurses to advocate on behalf of their patients, and to invest in training new nurses to address the current nationwide nursing shortage.
To discuss some of these issues, and to get a dose of real-life perspective on the profession, ScriptPhD.com sat down with Dr. Suzette Cardin, Assistant Dean of Student Affairs at UCLA’s venerable School of Nursing, ranked in the top ten of national nursing programs. Dr. Cardin has over 35 years of experience in nursing, and prior to her faculty appointment, she spent 14 years as Unit Director of the Critical Care Unit and the Cardiac Observation Unit at the UCLA Medical Center. She has been honored as a Fellow of the American Academy of Nursing and the American Heart Association. To read our interview, please click “continue reading”.
ScriptPhD: You have over 35 years of nursing experience. You’ve been in the trenches in the hospital, worked on the management side, and now are in academia training next generations of nurses. Safe to say, you’ve pretty much done and seen it all.
Suzette Cardin: Yeah, safe to say.
SPhD: In your opinion, what are the biggest challenges that the profession of nursing currently faces?
SC: I think the biggest challenge right now is to handle the [long-term] work force shortage with a large number of nurses getting ready to retire, and then a whole new workforce that will be replacing them. That, however, is being tempered with the fact right now that since we’re in a recession, the nurses who are scheduled to retire are not retiring. So that’s actually creating a double whammy in that the positions that people thought were going to be ready for students who were just graduating are actually not there. Because nurses have decided to stay and wait to see, waiting to retire is the problem. So that’s—the work shortage imbalance currently that we have. It was a year ago, we didn’t have enough nurses. But now we have too many nurses, because people haven’t retired due to the economic circumstances.
SPhD: Which is of course not a long-term solution, obviously.
SC: No.
SPhD: And I’m actually glad you brought it up, because my next two questions are completely pertaining to this. What are some of the reasons that nurses have been leaving the profession over the course of [the last few] years?
SC: I would say the main reason nurses leave is because they’re not happy with the work environment. So it could be related to the work conditions, it could be related to management style, it could be related to the type of patients that [they care for]. So, nursing is not what they thought it was going to be.
SPhD: Oh, I’m really surprised.
SC: What answer did you think I was going to give?
SPhD: I just thought it might have to do with the stress of the job over the course of however many years [they’re in the profession], or the aging population of current nurses. I didn’t realize that there was such a high level of dissatisfaction pervasive among the professionals.
SC: No, most nurses are happy. But there is a certain amount each year who leave their current jobs, go to another position because they’re not happy with the work conditions within. Now, there’s many professional organizations who have taken it upon themselves—The Association of Critical Care Nurses, and now here in California, the Association of Nurses–who have put out position papers on work conditions, and how does that work. They have seven or eight conditions that should be present in order for nurses to stay. The other important source of material is the magnet process, the magnet certification that hospitals undertake, in which there’s certain criteria, what they call “14 Forces of Magnet”, that institutes should have in place in order to be a magnet and attract nurses.
SPhD: We’ve listed some pretty dire statistics on the site with regards to nursing shortages, and stress levels on overworked nurses. There was a recent push on Capitol Hill [last month] to legislate mandated nurse/patient ratios to ensure patient safety, relieve workload and enhance quality of care.
SC: Which they already have in California.
SPhD: They do have that here in California?
SC: They have it in the ICUs and now they have it in emergency rooms and they have it on medical surgical units, they have it on OB/GYN. So, patients are classified according to an approved acuity system that’s acceptable and reliable. Then, based on that, they then assign high, medium, low acuity, and then you staff accordingly.
SPhD: But it seems like if you’re going to do it across the board, I mean the end goal is that nationally, regardless of what your status is as a patient, that for your benefit and for your quality of care it makes sense. You would have a certain ratio. But here’s my question. It seems to me, naively, you can’t just wave a magic wand and mandate that “You have to have a certain ratio of nurses to patients.” With such dire shortages and unchanging patient populations, what other fundamental legislative changes need to take place to rebuild the profession?
SC: I’m going to go on record as saying that I disagree with you, because we’re a profession, we have our own accountability and autonomy, and therefore we should be able to decide what is needed in what given situation. I don’t as a professional nurse like being mandated by the legislation that I need to do this in order to take care of patients.
SPhD: So you’re actually not a big fan of the mandated ratio legislation?
SC: No I’m not at all. I don’t like a group of lawmakers telling me what we should be doing that the force behind it is the Nurses’ Union. So I have very much a built-in bias [towards that]. What it does do is that it does assure patients that they will, based on their acuity and where they decide to be hospitalized, that they will get each nurse, say on a given unit may have four patients. But there’s no guarantee of the quality of those nurses. All it guarantees is that if there’s 32 patients on a nursing unit, and they each get four patients, that there will indeed be 8 nurses working that day. You have to assume the institution will guarantee the quality of those nurses. That’s just a given, but that’s not always the case.
SPhD: You’d mentioned these 14 forces of the magnet process that you have to have, etc. Extrapolating into the larger picture. Health care is hugely in the news right now. I know President Obama is going to a bunch of town meetings and we’re talking about health care reform. The health care system overall is broken in many ways. Surely, many of these overarching issues are tied together, i.e. it’s going to be tough to fix burdens nurses face without addressing uninsured patients or malpractice lawsuits or rising spending per patient or ERs closing around the country. These things seem to me to go hand in hand in the larger picture of health care overhaul. Is that a fair assessment?
SC: Yes, I think that’s fair. I think one of the reasons nurses leave [the profession] is because they get into it and they’re like, “Wow, this is really a mess.”
SPhD: Do you support a nationalized health care system, akin to Europe or Canada?
SC: I support a change being made. I’m not quite sure until I see what it looks like what I’ll support.
SPhD: Well, we’re talking somewhat within the context of Hollywood and medical show portrayal, which you had expressed concerns with in some of the emails we’d exchanged. What are the kinds of things that you see on television, film and the media, in terms of portraying what you do on a day to day basis, that frustrates you?
SC: Well, I think time and time again, the only people who can think are the physicians. The nurses are forever put in positions where thinking is not encouraged, we just do as we’re told, we’re the hand maiden to the physician. We don’t have a body of knowledge to make our decisions on. It’s kind of annoying. There’s a lot of jokes that are made about us. A classic one is [the television show] Scrubs. I mean, those nurses on that show are…. M*A*S*H was very good, in that it showed what nurses could do, however it was always at the expense of Hawkeye and his being a voyeur to nurses.
SPhD: You know, I think ER did a fairly decent job though, recently. Because Nurse Hathaway, who was the lead nurse of their unit, and a lot of the other nurses, were given a lot of respect and were shown working in concert with a lot of the other doctors. There was another example of fairly decent—sort of, kind of?
SC: Yeah, I wouldn’t say it was the best. Again, there was usually only one nurse highlighted that was always [working] about, and even the one nurse who ended up being highlighted, she ended up leaving to go to medical school.
SPhD: Right. Abby Lockhart, Maura Tierney’s character. When I watch medical shows, I have noticed a weird dichotomy. Either the focus is on doctors, in which case nurses seem to be these ephemeral accessories milling around in the background, or, if the focus is on nurses, they’re portrayed as somewhat antagonistic towards doctors (especially from the perspective of being book-smart versus street-smart). But in reality, wouldn’t that relationship have to be by nature synergistic to best serve patients?
SC: Well, it doesn’t reflect what actually goes on in practice. I would say the best example that I’ve ever seen was over at UCLA in the medical ICU. They would go on rounds in the morning, of course these were teaching rounds, but the nurse would have her say, the resident intern who was caring for the patient would say what was going on, and believe it or not the family member would also say and be able to ask questions. And the respiratory therapist was there, the pharmacist was there, I mean the whole team was there and everyone had an equal say with what was going on in the patient.
SPhD: And a lot of times you find that nurses are the vasculature of a hospital, ensuring that a patient’s day-to-day needs are being taken care of. So it makes no sense that they wouldn’t be involved on a higher level of patient care.
SC: Right. Right. So that to me is an excellent example of good synergy and people working together as a team.
SPhD: What are some key stories or issues that you would really like to see portrayed or addressed more in media and popular culture?
SC: Well, that example. That when information is given to patients, the patient is there, the family is there, all the health care team members are, everyone is incorporated into what’s going on, the nurse does more than just report what’s going on, they come up with the plan, this is what I see going on with the patient, I was thinking about this, what do you think, they kind of go back and forth. [It’s an] equal exchange of ideas.
SPhD: That ultimately medical care has a lot more synergy than is currently being portrayed. It’s not so compartmentalized.
SC: Exactly.
SPhD: We just had a slew of graduations here on campus and the UCLA Nursing program is a nationally renowned program. You guys regularly produce the best and brightest nurses in the nation. To a graduating nurse that is about to join the workforce, what is your advice?
SC: To be as open and flexible as they can in how they view the current health care system, to realize that change is going to occur and to go with the flow, they’re not all going to get the jobs they want, just because there’s now a scarcity of jobs. That’s going to be—we have a group of students who just graduated, who two years ago when they came [to UCLA], we said, “You are going to get any job you want.” Now they’re going around and scrambling around to get jobs. Not all of them have jobs, not all of them are going to get jobs, so that’s been really difficult in the last six months. Maybe they will have to get creative. With that I just think they need to be open-minded, be flexible, be adaptable.
SPhD: That’s excellent advice. I just wanted to on a personal note say that a lot of the stuff we talked about highlights problems that exist or dissatisfactions, but having been a patient numerous times, personally, I have yet to encounter a nurse that is not nurturing, caring, deeply passionate about his or her job and I just want to say on the record, on the ScriptPhD site, from me personally, that I think there is something so intrinsically nurturing about this profession. So thank you so much, for meeting with me and for what you do!
SC: Oh you’re welcome!
~*ScriptPhD*~
]]>